50 year old with recurrent hypoglycemia
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
DR. JAYANTH ( INTERN)
DR. AMULYA ( INTERN)
DR. SURYA PRADEEP ( INTERN)
DR. ASHA KIRAN ( INTERN)
DR. YAMINI ( INTERN)
DR. VAMSHI ( INTERN)
DR. ISMAIL (INTERN)
DR. PRADEEP ( PG 1st YEAR)
DR. NIKITHA ( PG 2nd YEAR)
DR. SUFIYA ( PG 3rd YEAR)
DR. SATISH ( PG 3rd YEAR)
Faculty : DR. VIJAYALAXMI
Here is the i have seen-
50 year old female came to casualty in unresponsive state E1V1M2 (GRBS-24mg/dl) one 25D was connected and then the patient became responsive within 15min.
Patient C/o-
1. Fever since 3months.
2. Burning micturition since 15days.
3. Vomitings since 10day.
4. Generalized weakness since 10day.
Patient was apparently alright 3months back then she had fever which was insidious in onset, intermittent type, not associated with chills and rigors. Relieved on taking medication.
One episode of vomiting /day which is non-projectile and non-bilious with food particles as the content since 10days.
No h/o loose stools, pain abdomen, headache, blurring of vision, chest pain, palpitation.
PAST HISTORY-
K/C/O DM II since 10years on HAI
8U------x------7U since 1 year.
K/C/O HTN since 7years.
Similar episode of hypoglycemia 1year back for which she was admitted in our hospital only and stayed for 10days.
Not a K/C/O asthma, TB, CVD, epilepsy.
PERSONAL HISTORY-
Her appetite is normal and is a non vegetarian with regular bowel and bladder movements.
No known allergies.
GENERAL EXAMINATION-
Patient is c/c/c.
Moderately built.
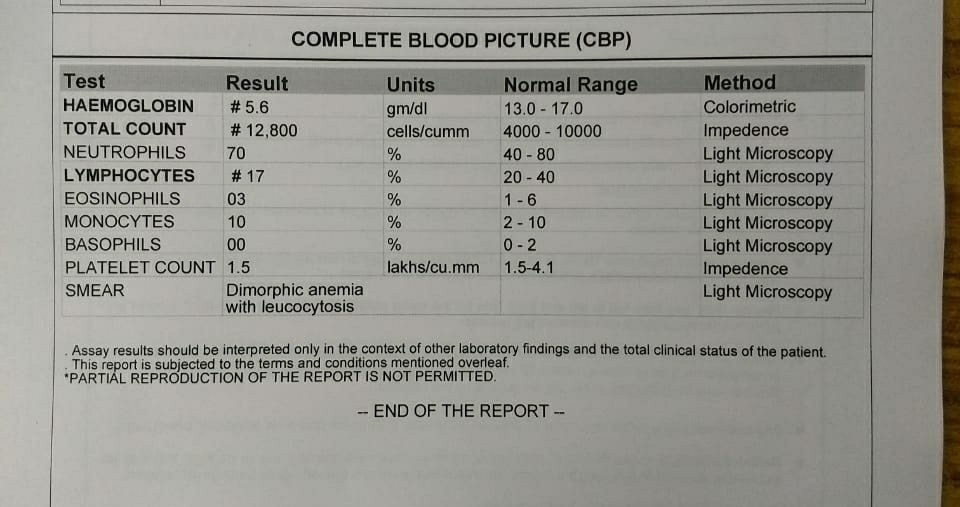
Pallor is present.
No signs of icterus, cyanosis, clubbing, lymphadenopathy, pedal edema.
Vitals-
Afebrile to touch
BP-150/100 mmhg
PR- 75/min
RR- 18cpm
Spo2- 98% on RA
GRBS- 24mg/dl------>331mg/dl with25D
SYSTEMIC EXAMINATION-
CVS- S1 S2 present, no murmurs and no thrills
RS- BAE present no added sounds
PA- Soft, NT, no organomegaly.
CNS- Patient is concious with normal speech, no signs of meningeal irritation, no deficits in cranial, motor, sensory systems.
GCS-E1V1M2------>E4V2M4 after 25D infusion.
PROVISIONAL DIAGNOSIS- RECURRENT HYPOGLYCEMIA SECONDARY TO ?SEPSIS WITH AKI ON ?CKD WITH K/C/O DM II.
TREATMENT-
ON DAY OF ADMISSION 16/02/2021
1. IVF NS and RL u.o+30ml/hr.
2. IVF 25% DEXTROSE.
3. Strict I/O charting.
4. GRBS hourly monitoring.
5. Inj. NaHCO3 50mEq IV STAT.
Inj. NaHCO3 50mEq IV in 199ml NS over 30min to 1 hour.
ON DAY 1- 17/02/2021
S-
C/O burning micturition.
No fever spikes.
O-
Patient is c/c/c.
Afebrile to touch.
PR-78bpm
RR-20cpm
BP-150/100 mmhg
CVS-S1 S2 present
RS-BAE+ NVBS
PA- NT, Soft
A-
RECURRENT HYPOGLYCEMIA SECONDARY TO ?SEPSIS WITH AKI ON ?CKD WITH K/C/O DM II.
P-
1. IVF 2units NS and 1unit RL- urine output + 30ml/hr.
2. Inj. PANTOP 40mg IV OD.
3. Inj. PIPTAZ 4.5 gm IV STAT
Inj. PIPTAZ 2.25gm IV TID
4. GRBS hourly and inform if <100mg/dl or >250mg/dl.
5. Strict I/O charting.
6. BP/PR/Temp hourly.
7. T. AMLONG 5mg PO OD.
8. Withhold insulin until further orders.
9. Oral fluids upto 2L/day.
10. Inj. RANITIDINE 50mg IV BD.
TREATMENT on day 2-18/02/2021
S-
Burning micturition decreased.
No fever spikes.
Stools passed and pedal edema decreased.
O-
Patient is c/c/c.
Afebrile to touch.
PR-92bpm
RR-20cpm
BP-130/80 mmhg
CVS-S1 S2 present
RS-BAE+ NVBS
PA- NT, Soft
CNS-HMF intact, no FND.
A-
RECURRENT HYPOGLYCEMIA SECONDARY TO ? UTI WITH AKI ON ?CKD WITH K/C/O DM II.
P-
1. Inj. PIPTAZ 2.25gm IV TID
2. GRBS 4th hourly and inform if <100mg/dl or >200mg/dl.
3. Strict I/O charting.
4. BP/PR/Temp hourly.
5. T. AMLONG 5mg PO OD.
6. Oral fluids upto 2L/day.
7. Inj. RANITIDINE 50mg IV BD.
TREATMENT on day 3-19/02/2021
S-
No fresh complaints.
O-
Patient is c/c/c.A
Afebrileto touch.
PR-68bpm
RR-19cpm
BP-110/70 mmhg
CVS-S1 S2 present
RS-BAE+ NVBS
PA- NT, Soft
CNS-HMF intact, no FND.
A-
RECURRENT HYPOGLYCEMIA(RESOLVED) SECONDARY TO ? UTI WITH AKI ON ?CKD WITH K/C/O DM II.
P-
1. Inj. PIPTAZ 2.25gm IV TID
2. GRBS 6th hourly.
3. Strict I/O charting.
4. BP/PR/Temp hourly.
5. T. AMLONG 5mg PO OD.
6. Oral fluids upto 2L/day.
7. T.RANITIDINE 150mg PO OD.














Comments
Post a Comment